Adapted microfluidic device design sheds light on invasive lines of cancer cells
A team of researchers from the University of Michigan Comprehensive Cancer Center (MI, USA) have developed a tiny microfluidic device that could detect and distinguish early cancer aggressors, whilst also identifying opportunities for intervention to prevent metastasis.
Sofia Merajver (University of Michigan Comprehensive Cancer Center) stated: “It’s especially important to be able to capture those leader cells and understand their biology — why are they so successful, why are they resistant to traditional chemotherapy and how can we target them selectively?Microfluidic devices are helping us understand biology that was previously not accessible.”.
Currently, cells struggle to survive for long periods of time in microfluidic devices and are therefore limited to brief experiments lasting only a few days. Whilst these experiments have proved useful in the past, the changing characteristics of cancer cells, over longer periods of time, have not been able to be studied.
“A lot of tumor processes like invasion and resistance don’t happen overnight. Our goal was to track the long-term evolution of invasion. We cannot look at just a certain time point, like in a three-day experiment. That might not represent what’s happening in the body over time,” commented Koh Meng Aw Yong (University of Michigan Comprehensive Cancer Center).
New research, published in Scientific Reports, has provided an answer to lengthier incubation times, and therefore allowed valuable insights into the changing characteristics of cancer cells. The new design enables the microfluidic device to maintain stability for up to 3 weeks in culture.
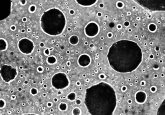
With cells suspended three dimensionally in the chamber, the microfluidic device is different from standard microfluidic devices, which typically capture cells over two dimensions. This allows minimal disturbance or change to the cells as researchers feed cancer cells into the device.
Three tiny molded channels make up the device. The cells are fed into one channel and fluid flows through a parallel channel providing pressure and flow with minimal disturbance to the culture. Fluid flowing through the third channel mimics blood capillaries.
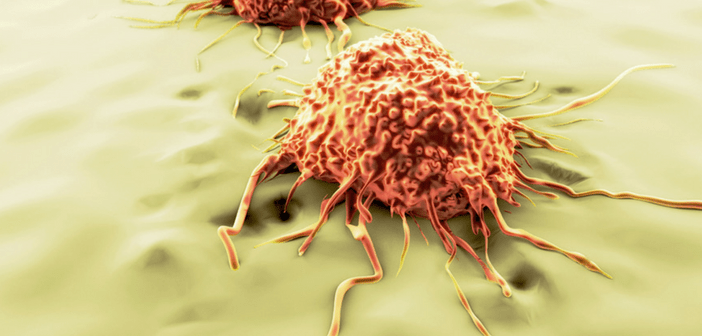
The study involved tracking two lines of metastatic prostate cancer cells. The main cells of focus were leader cells, which are the first cells to break off and hypothetically travel to alternative organs. Through using the newly design microfluidic device the team were able to isolate these leader cells.
Researchers also demonstrated differences in the invasive properties of the two lines after 2 weeks, but this decreased after week three suggesting a time-related change in invasive potential over time. If researchers can differentiate between the molecular signatures of invasive and non-invasive cells, there could be potential in the development of therapies targeting invasion, keeping the cancer confined and preventing metastasis.
On discussing the future application of this research, Jianping Fu (University of Michigan Comprehensive Cancer Center) commented: “The device also holds potential to be used to test drugs and detect when cancer becomes resistant. This would allow oncologists to know sooner if a therapy is not working, and perhaps switch the patient to another option. Of course, more research is needed to explore this possibility in the future.”
“We think we can grow this while the patient is undergoing treatment or monitoring. The device would be able to show us if the cells become more aggressive before a traditional imaging test would detect anything,” Aw Yong added.
The next step for the team is to extend this study to highly aggressive triple-negative breast cancer. With research again focusing on leader cells, the team will begin to look for differences between the genetic and molecular markers of the most and least invasive cells.
Sources: Aw Yong KM, Li Z, Merajver SD & Fu J. Tracking the tumor invasion front using long-term fluidic tumoroid culture. Sci. Rep. 7 doi:10.1038/s41598-017-10874-1 (2017); www.sciencedaily.com/releases/2017/09/170907093654.htm