Picking up the warning signs for type 1 diabetes
Frequent dried blood spot microsampling of protein markers shows promise for timely intervention for type 1 diabetes.
Dried blood spot sampling (DBS) — a type of microsampling whereby small droplets of blood are dried onto filter paper card — has been used to track predictive markers of type 1 diabetes in mice. The team, based across the Karolinska Institutet, KTH Royal Institute of Technology and SciLifeLab (all Stockholm, Sweden), demonstrated that analyzing minute amounts of blood at regular intervals can reveal disease-causing changes, potentially enabling early treatment and disease prevention if translated to human studies.
Type 1 diabetes is an autoimmune disease whereby the immune system attacks the insulin-producing beta cells in the pancreas, reducing insulin production. Often developing gradually, the biological changes indicating type 1 diabetes can be difficult to detect. In 95% of people who develop the condition, approximately 6 months to 2 years before disease onset, islet-reactive autoantibodies appear, acting as a warning for type 1 manifestation. Previous studies have identified serum proteome changes that are linked to the appearance of these antibodies or the onset of type 1 diabetes, but proteome profiles have not yet been correlated with a disease-triggering event.
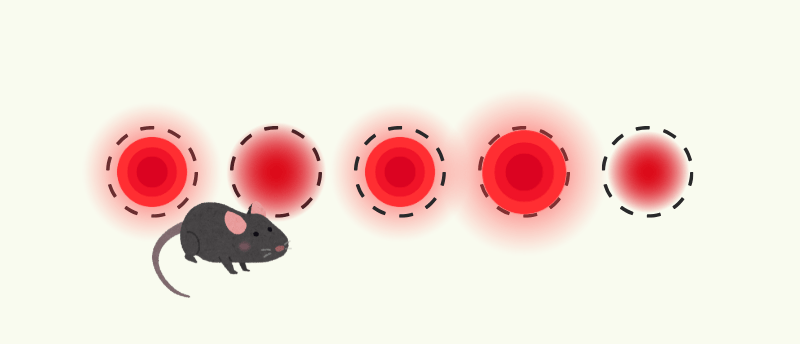
In this new study, the team investigated whether frequent blood microsampling in mice post infection with Coxsackievirus, a virus suspected of triggering type 1 diabetes, could reveal these changes at an early, presymptomatic stage. The study investigated whether blood microsampling and affinity-based proteomics could capture changes in the circulating proteome that are induced by a disease trigger and whether this could inform timely, molecularly-informed interventions.
Over a 2-week period, blood samples were taken at regular intervals and stored as small, DBS samples. The Olink Target 96 Mouse Exploratory panel was used to measure 92 circulating proteins from the elutes of these spots, which were assessed by proximity extension assays. The results of this study showed that frequent blood sampling and longitudinal measurement of the blood proteome revealed transient molecular changes in virus-infected animals, which, with less regular sampling, would have been missed.
You may also be interested in:
- Quantitation of BCAA and BCKA in plasma and patient-centric dried blood microsamples in a clinical setting
- In the Zone: the importance of tailored sample preparation methods
- Catching COPD before it starts
“Our hope is that this cost-effective technique, which involves taking small samples of blood that are dried and stored at room temperature, can be used for regular testing at home. This would make it easier to monitor the progression of the disease in people who are at high risk of type 1 diabetes,” says Malin Flodström-Tullberg, Professor at the Department of Medicine, Karolinska Institutet.
The researchers were also able to predict infection status 2 days after delivery of the virus with over 90% accuracy. This early detection meant that treatment of infected individuals with immune sera on day 2 prevented type 1 diabetes development in 100% of cases.
Not only does this study demonstrate the utility of DBS samples to measure dynamic proteome changes that could be translated to human initiatives, it also represents a significant step towards reducing the number of animals needed for laboratory research and improving the welfare of those animals needed for studies.

