3D imaging technology improves diagnosis accuracy for basal cell carcinoma
Cases of basal cell carcinoma (BCC), the most common form of cancer globally, have doubled in the last two decades alone. Early diagnosis, involving subtype classification of BCC, is necessary for effective treatment and reduced morbidity. Researchers from the Department of Dermatology at the Hôpital Erasme, Université Libre de Bruxelles (Brussels, Belgium), have developed a novel imaging technique to improve the diagnosis accuracy of BCC by 12%, reducing the need for unnecessary biopsy surgeries.
Although BCC is a slow-growing form of cancer unlikely to spread, in Europe, skin cancer affects 50 –80% of people each year. This rate has doubled in the last 20 years, which is generally attributed to sun exposure and the use of tanning beds.
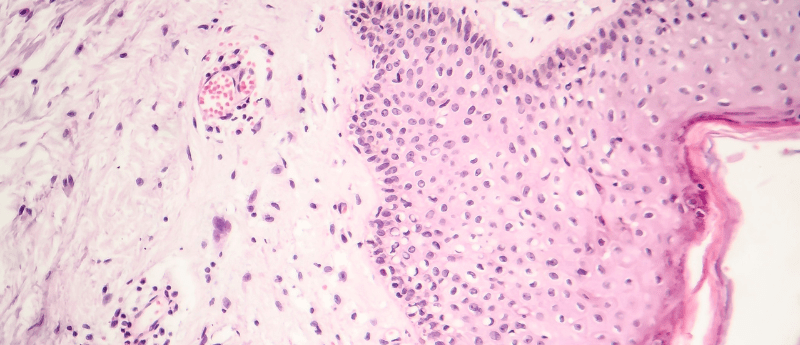
Typical skin cancer diagnosis relies upon the use of traditional dermoscopic examination of skin lesions to determine the cancer subtype – such as superficial BCC, a BCC-imitator like squamous cell carcinoma, actinic and seborrheic keratosis, dermal nevus, or inflammatory conditions, or other BCC subtypes. This differentiation is crucial for clinicians to determine which treatment to pursue with a patient.
You may be interested in:
- 3D imaging solutions to support pre-clinical drug discovery
- Worm your way to diagnosis: ‘worm-on-a-chip’ device could be used to diagnose lung cancer
- Minimally invasive and highly accurate liver fibrosis test
New research presented at the 31st European Academy of Dermatology and Venereology conference (7-10 September, Milan) by the research team at the Department of Dermatology at the Hôpital Erasme has shown that BCC diagnosis accuracy can be significantly improved by using line-field confocal optical coherence tomography (LC-OCT). LC-OCT provides detailed 3D imaging at the cellular level, whereby a light beam from a supercontinuum laser is used to illuminate the skin.
The interaction of this light with the microstructures in the skin lesions creates backscatter and the amplitude and echo-time delay are then detected by the line-scan camera. This data produces 3D images in real-time of the skin lesions, allowing for distinct morphological features to be identified, leading to BCC subtype diagnosis.
Analysis of 303 lesions which contained 173 BCC and 130 BCC-imitator samples indicated a 12% increase in diagnostic accuracy when using LC-OCT before surgical excision, when compared to the use of dermoscopic techniques alone. Integration of LC-OCT improved BCC diagnosis accuracy from 85% to 97%, whilst the differentiation between superficial and non-superficial BCC accuracy increased from 80% to 92%.
Mariano Suppa, lead researcher and consultant dermatologist, commented:
“LC-OCT has the potential to reduce the number of unnecessary biopsies and excisions in cases of superficial BCC and also in the case of benign lesions that do not require surgery”.
The research team also produced a diagnostic algorithm to aid clinicians in diagnosing different BCC subtypes. The algorithm is based upon the most influential morphological criteria from the statistical analysis of the LC-OCT data collected.
Suppa believes this research signifies a major improvement in the diagnosis and treatment of BCC:
“Diagnosing basal cell carcinoma can be challenging using clinical or dermoscopic assessments alone and the condition must be correctly diagnosed in order to treat it properly. We found that the accuracy of diagnosis can be improved by at least 12% using LC-OCT, both in terms of differentiating BCCs from other skin conditions and of identifying BCC subtypes that do not require surgery”.
Source: Eureka press release: https://www.eurekalert.org/news-releases/963771