NHS centre opening in the UK for revolutionary cell and gene therapies

NHS Blood and Transplant (NHSBT) is opening a state-of-the-art facility today, which will contribute greatly to the UK’s ability to develop and manufacture new gene and cell therapies.
It will manufacture products for the development of potentially curative therapies for currently incurable diseases, such as some forms of cancer, sickle cell disease and cystic fibrosis. Some of these will be personalised therapies, which will be aimed at treating just one person.
The latest Clinical Biotechnology Centre (CBC), built in Bristol with the help of a £10m government grant, aims to expand the UK’s ability to make clinical-grade products required for the research and development of new cell and gene therapies.
Steve Barclay, Health and Social Care Secretary, stated:
“The government is backing new gene and cell therapy which uses living cells or genetic material such as DNA to cure diseases. […] The investment in this new centre will continue to develop this area of research and help provide patients with the best possible care. […] We announced our ambitious Life Sciences Industrial Strategy to tackle cancer and life-changing illnesses and ultimately save lives. […] This works best when we work collaboratively and this new centre is the perfect example of the government, NHS and those in research and manufacturing collaborating to eventually deliver new transformative treatment to NHS patients.”
This centre will help support early-phase clinical trials and pre-clinical work, providing a route to eventual commercial-scale production. It will help patients gain quick access to the latest treatments, by including more UK patients with incurable diseases participating in clinical trials and bringing new treatments into the NHS faster.
Cell and gene therapy is a cutting-edge area of medical development. Therapies are based on the idea that living cells or genetic material can be used to cure a wide range of acquired and inherited diseases, by altering their DNA or using them as a vehicle to deliver treatments. Gene and cell therapy can be used to treat illnesses such as leukaemia, haemophilia, autoimmune disorders, cancer, HIV, melanoma and cystic fibrosis.
Somebody who has benefited from cell and gene therapy treatment is Nitya Raghava, 22, from Gloucester, who had lifesaving CAR-T cell therapy for acute lymphoblastic leukaemia and who will speak at the centre opening today.
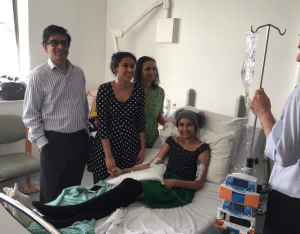
She was diagnosed through blood tests in 2016 after experiencing more than a month of fevers and headaches. Nitya had treatment including chemotherapy and a stem cell transplant but after a relapse, CAR-T was ‘pretty much a last resort.’ Nitya went on to become the first person to receive CAR-T therapy at the Bristol Haematology and Oncology Centre in February 2019. Nitya has now been free of the disease for four years. She said:
“I felt really excited to be able to receive CAR-T cells given they were new to the NHS. CAR-T was absolutely lifesaving for me. Without it, I don’t think I would be here. I think it’s just so exciting to see other new cell and gene therapies being developed at the CBC that can help other people too. I now feel great, I’m at university and I am living my life as normal. four years on from receiving CAR-T cells, because I’m in complete molecular remission with no evidence of disease now. I feel lucky that I got it when I did, and I hope more people also now get the chance to have new treatments. I hope the new CBC can help other new treatments to reach patients faster.”
Such advances in biotherapies offer new hope for patients for whom all other treatment options have been exhausted. CAR T-cell therapies have now been used to treat hundreds of patients. The CBC has been built at NHSBT’s base (Bristol, UK) to replace the smaller unit in nearby Langford. Larger commercial sites do exist, which are cost-effective for making products for proven treatments. However, researchers need access to flexible sites where they can make smaller amounts for treatments still being researched and clinically tested cost-effectively, which is what the CBC will specialise in.
Currently, the UK has limited capacity to make the DNA plasmids and viral vectors, used in the manufacture of gene therapies and genetically modified cell therapies. In particular, there is insufficient manufacturing at the scale required by organisations wishing to undertake early-phase clinical trials of these biotherapies. The shortage of UK manufacturing capacity means increased delays for the developers of gene therapies while they wait for production slots. Researchers often need to seek the services of overseas manufacturers, which inevitably delays clinical trials and patients’ access to much-needed innovative therapies as well as often increasing costs. The new CBC will change that by expanding the UK’s ability to make its own plasmids and viral vectors.
Expanding and improving the CBC’s unique offering is in line with the Government’s Life Sciences Industrial Strategy, which is to grow the UK’s manufacturing capacity for DNA-based therapeutics.
Finally, Lilian Hook, Director of Cell, Apheresis and Gene Therapies at NHSBT commented:
“The CBC is basically a factory – it manufactures the building blocks (or components) needed to produce gene therapies. Researchers and developers can ask us to manufacture the specific components they require. This will enable cutting-edge research with the potential to develop cures for some critical diseases which can currently only be treated and often ultimately prove fatal. We’ll be supporting the delivery of these curative treatments into the NHS, so patients can access them more quickly. The CBC will help the UK grow its cell and gene therapy industry in a rapidly growing international market. We won’t be designing the treatments but we will be manufacturing them to the right scale and clinical grade. Cell and gene therapy is a growing area for the healthcare sector and part of our direction of travel as an organisation.”